It’s all alphabet soup in the end
So Johnson & Johnson have submitted their data to the FDA for emergency use authorization (that’s EUA for those of you who speak alphabet soup). The data on this one are super interesting, so I’m going to talk about some new things we know!
What is an EUA, anyway?
An Emergency Use Authorization means that (1) an emergency exists involving some kind of serious or life-threatening health condition (it is all alphabet soup here) (2) there are no traditionally-approved treatments for this condition (3) the FDA have reviewed the existing data on an intervention (could be a procedure, a medication, a device, etc) and it looks like it might have a benefit even though the full criteria for FDA approval have not been met.
Sometimes, later information comes out that makes it clear that the intervention is not, in fact, helpful, and the EUA gets revoked. We have seen that several times with this pandemic – with certain COVID tests, with certain medications, and even with certain kinds of personal protective equipment. The FDA continuously evaluates the information that’s available to them.
What manufacturers are hoping for, of course, is that the long-term data will support full FDA approval in the end. An EUA is not a shortcut to approval – it’s a tool that we have to use when lives are at stake and we can’t afford to wait for the usual (potentially years-long) process to grind along.
What about the Johnson and Johnson vaccine?
J&J applied for EUA for their vaccine on Friday. It’s a single-dose adenovirus vector vaccine (they are still running trials on a 2-dose version), so this vaccine works a little differently than the two vaccines currently on the market. Basically, J&J are using an adenovirus – a particular type of virus that’s really good at getting the body’s attention, thanks to the fact that they infect pretty much everybody (this is another common cold-causing virus) – and have modified it so that it’s not so good at actually copying itself any more. What it does do is present a set of instructions to the cells (just like the mRNA vaccines) to make viral spike proteins.
This vaccine uses DNA — so it depends on the body to translate the instructions for making spike proteins into mRNA and take them to the factories. It can’t actually affect the DNA that’s inside your cells already (and neither can the mRNA vaccines); it simply doesn’t have the enzymes to unzip your cells’ DNA and break it apart.
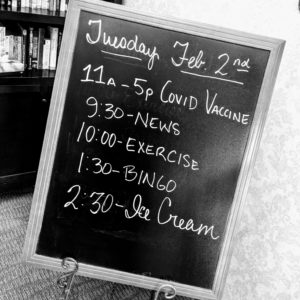
J&J enrolled a little over 43,000 people in their global trial, and saw 468 symptomatic cases of COVID-19 in that trial. They designed the study to look for moderate to severe COVID-19 at 14 and 28 days after vaccination, as well as for all symptomatic infections. They also did genetic tracking on the types of COVID-19 infections they saw.
So what did they find? A couple of interesting things.
The vaccine was 66% effective in preventing moderate to severe COVID-19 at 28 days after vaccination — and there was enough data to say that in the US, it’s more like 72%. That’s not as good as the 94-96% prevention that Pfizer and Moderna have reported, but it’s still pretty substantial; about as effective as the adult pneumonia shot (Pneumovax23 in the US). There’s a bit of more important information in the report, though: J&J reports no cases of COVID-related hospitalization or death after day 28 in the vaccinated group.
This is a vaccine that protects people. It’s a good vaccine!
It may not be quite as amazingly amazing as Moderna and Pfizer’s prevention numbers (although preventing hospitalization and death is a BIG deal), but it has pretty solid safety information: there were no cases of anaphylaxis reported during the trials, and the placebo arm reported higher rates of serious adverse effects than the active vaccine arm. J&J notes that this is actually not the first vaccine candidate using this technology (their Ebola vaccine was actually approved in Europe in 2020), and that they’ve seen similar safety profiles in those long-term trials. This is a vaccine whose driving technology has a longer-term track record.
This vaccine also has some ability to see through a false nose and sunglasses! It’s not perfect; it did show decreased efficacy against the South African variant B.1.351 (remember: this variant coronavirus is super friendly AND doesn’t quite look like its wanted poster), but still protected people about half the time. That’s not bad! It’s about as good as the old shingles shot was for shingles prevention (the new one is almost 90%).
We have some pre-print data that suggests Moderna and Pfizer’s vaccines work to neutralize the mutant viruses in test tubes — but humans are not test tubes, pre-print data still needs outside eyes to look at it, and so we don’t know what the real-world effects will be.
And this is where I remind you that variant B.1.351 has been seen in the United States, and this is why — even when you’re vaccinated — it’s still important to wear your mask, keep your respectful social distance, and avoid spending time with groups of people indoors, especially if there is eating and drinking involved.