I am a process nerd.
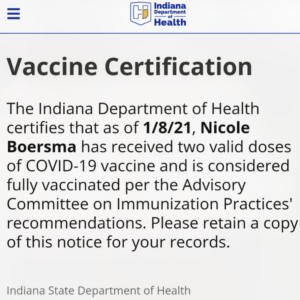
I had a migraine this morning, but I am prepared to blame it on a combination of staying up until 1 AM playing Dungeons and Dragons and waking up to snow all over the ground this morning. From a vaccine standpoint, I have no complaints.
In case you missed my Wednesday midday post, Indiana has opened their vaccination program to ages 70 and up! The Department of Health was not quite prepared, I think, for the number of registrations they received: my news alert at noon on Thursday reported that more than 250,000 Hoosiers ages 70 and older had already scheduled appointments, and many people are reporting long wait times through the 211 helpline. That’s exciting news but also highlights the immense amount of coordination and infrastructure support that is needed to perform mass vaccination (something your public health departments help to coordinate on an annual basis in flu vaccine season).
A little talk about vaccine storage
The CDC has updated their current recommendations for vaccination to include people ages 65 and over as well as those under 65 with high-risk health conditions, but some parts of the country hospitals and health systems are still struggling to get enough supply to vaccinate their workers – while in other systems, calls are going out at the end of the day to avoid wasting already-drawn vaccine doses due to no-shows or appointments being left unscheduled. That’s a problem.
There are a lot of factors that play into the supply and demand equation here, and supply-chain logistics is not something that I’m prepared to write a blog post at this time (also: that discussion is Fraught with complexity beyond my skill level). I’m also not prepared at this time to engage with the larger discussion of “who should get vaccines first,” because that is also Fraught. But one of the aspects I am prepared to talk about is the delicate timeframe we’re playing with here, and why we can’t just put the syringes back in the refrigerator for tomorrow.
Remember, both of the current vaccines are mRNA vaccines, and RNA is very fragile. Both Pfizer and Moderna have wrapped that RNA up in lipid nanoparticles (that’s little fat bubbles, for those of you playing the ‘plain English’ game), and in order to keep the whole thing from just falling apart into a tiny greasy mess it has to be kept super cold.
Pfizer’s vaccine is the fiddliest: it’s good in an ultracold freezer (-70°C/-94°F) for 6 months, on dry ice (replaced every 5 days) for a month, and in a hospital refrigerator for 5 days. Moderna’s vaccine is much easier to store – it can stay in a regular freezer until its expiration date, instead of Pfizer’s ultracold one, and lasts thawed for 30 days in a hospital refrigerator. For both vaccines, once the vial is punctured and you mix it for administration (at room temperature) it’s good for six hours. You can’t go backwards – once the seal is broken those doses have six hours to be given or they’re lost as the mRNA degrades.
That’s a problem, and one there really isn’t a good way to solve other than keeping those “call lists” and reminding people to hang on to their vaccine appointments. These vaccines just aren’t built to sit around, and Pfizer’s candidate especially requires a special ultracold freezer to store it. That’s a huge investment — and when we start talking about hardware requirements to distribute a vaccine, we start talking about disparities of distribution (which is another post in itself).
There’s a new kid strolling casually onto the block, though: Johnson and Johnson (referred to as J&J for the rest of this post) have announced some preliminary results of their phase 1/2a studies just this Wednesday, and they are seeing neutralizing antibodies in 90% of recipients at day 29 after the vaccine, with 100% of recipients showing neutralizing antibodies at day 57 and antibodies lasting to day 71 (that’s the last day they took data before publishing). This one-shot adenoviral vector vaccine is probably going to be stable in a regular freezer (-20°C/-4°F) for 2 years and refrigerated for more than 3 months.
Let’s break down the science talk on that, shall we?
I talked in an earlier post about how an mRNA vaccine works (10-second recap: mRNA is a set of instructions for your cells to print their own Wanted posters with the image of a particular part of the coronavirus spike protein), and that’s how both Pfizer and Moderna vaccines work. The J&J candidate is an adenoviral vaccine instead. It’s built on the technology that J&J (operating as Janssen Pharmaceuticals, their R&D arm) used to produce their Ebola vaccine, which has been in development since 2014 and was approved in Europe earlier this year.
Adenovirus vaccines use an actual virus that has been heavily modified so that it can no longer use humans to make a zillion copies of itself (remind me sometime and I’ll talk about the crazy things that viruses do inside your cells). The adenovirus itself is just a string of DNA wrapped in a package of proteins called a capsid, which is the part the immune system sees. Human immune systems are equipped to produce a robust response to adenoviruses in general. As a viral researcher, that means I can stick some easily-recognized parts of the virus I *actually* want the immune system to destroy into the capsid, and count on your immune system going bananas about it.
Specifically, the participants in J&J’s trial are showing the development of neutralizing antibodies in every participant within 2 months after a single shot. Neutralizing antibodies are the blockers of your immune system. They grab onto viruses and prevent them from infecting cells in the first place, so this is a genuinely promising result from technology that’s been under development for quite a while and has already been successfully used in another vaccine.
This data is also just the Phase 1/2a preliminary data, which is a great excuse to talk about how clinical trials work, the importance of blinding, and why things seem to be moving so very swiftly these days!
What’s up with the speed of vaccine trials and the Emergency Use Authorization? Can I really trust this information? Everything is happening so fast!
The short answer is: we have rearranged the way trials are structured and allowed for a temporary authorization based on the data that’s available at this point; all of this is still being studied so it’s important to participate in post-vaccine monitoring.
This is a SUPER LONG READ.
Traditionally, when you have a new therapy (a drug, a vaccine, or some cool intervention) that you think will be effective for treating a disease, you perform human trials (after all the preliminaries) in four phases. Each phase is independently structured, and researchers fully complete one phase before moving on to the next.
Phase 1: Safety. A small group of volunteers who understand that the thing you are doing to them is hopefully-but-not-definitely safe are given gradually increasing doses of your drug-or-vaccine. Samples are taken to look at blood levels, where appropriate. Participants are closely monitored for toxicity. The goal of Phase 1 trials is to answer the question “What is a safe dose range for this drug?”
Phase 2: Efficacy. A larger group of volunteers are divided into a “control” and several “interventional” arms. The control volunteers are given a placebo (in medication trials, this is a sugar pill; in vaccine trials it can be a saline solution), while the interventional volunteers are given possibly-but-not-definitely effective doses. The goal of Phase 2 trials is to answer two questions: “How much drug should be given?” (Phase 2a) and “Does this drug work at all?” (Phase 2b).
This is where J&J have currently stopped. They’ve released the results of phase 1 (safe dose range) for and 2a (effective dose) for all trial participants, but they are still doing some data analysis in their 65+ participants. That’s expected at the end of January. The conclusions drawn from the data we have available from the trial at this point are:
- This vaccine appears to be safe
- The dose used appears to be effective at inducing an immune response.
We are pretty sure that – given the antibodies being measured – the vaccine will be effective, but we can’t say that for sure because that data hasn’t been released. That’s the Phase 2b question.
One of the ways vaccine manufacturers have saved time is by combining phases 1 and 2 or phases 2 and 3, depending on the information that’s already available. That means they’re running multiple studies simultaneously based on “best guess” numbers (J&J is actually still collecting data on whether a 2 dose series will be better than a 1 dose protocol, for example). That saves time.
Once Phase 2a and 2b are completed, trials move into Phase 3, which is the large clinical trial phase. In medication trials, the experimental medication is compared to existing therapies; in the coronavirus vaccine trials the experimental vaccine is compared to a saline injection (because there is no existing therapy). Again, the experimenters and the participants are “blinded” — who gets the treatment and who gets the placebo is kept secret — because this phase is designed to answer the question “What can we expect in the real world?”
This is the part where the statisticians get involved, because things happen in the placebo arm of a trial too. People in both arms of a phase 3 clinical trial are still people, and they are still going about their daily lives, with a range of experiences that affect their health and well-being. In a well-designed trial, your statistician has suggested enrollment numbers that should help your trial take all of these things into consideration. Your statistician has also helped you set an interim analysis point (more on this in a minute).
People who are enrolled in a clinical trial are being monitored for any and every side effect they choose to report. They are also being monitored for evidence of the *endpoints* of the trial (in the coronavirus vaccine trials, this has generally been “did you get symptomatic COVID-19?”) Those reports are then handed to statisticians, whose job is to break down the reports and answer two questions: “Did this event happen *a meaningful number of times* more often in the intervention arm than the placebo arm?” and “Did this intervention accomplish the goal *in a meaningful way*?”
We have computers to help with those analyses, thankfully. Even more thankfully, we have statisticians who are trained to select the right analysis for the problem, because even though math itself is pretty cut and dried, choosing the math you do can make a dramatic difference in the appearance of the final results.
Phase 3 clinical trials traditionally last for quite a long time! Because of this, researchers can set an interim analysis point in their trials: This is a point where they can step back, take a look at the data, and decide if the information they have is *overwhelmingly* in favor of the intervention they’re testing. In that case, they may decide to stop the trial early (so everyone can get the benefit of the intervention) and continue analyzing data in Phase 4 (the part where we continue to collect data after a drug or intervention is released to the market).
That’s what happened with the Pfizer and Moderna trials, and what J&J hopes will happen in their trial: the interim analysis showed an overwhelming benefit in favor of vaccination (with regard to symptomatic coronavirus infection) and so the decision to move for Emergency Use Authorization was made. It means that we don’t have as much data as we normally do from a clinical trial, though, so it’s a decision that should not be made lightly. It’s also a decision that ideally is made based on pre-established criteria (remember when I said it was super important that the trial protocols were made public in advance?) so that the decision is not influenced by the hopes of the researchers.
We all have skin in the game when we do something; one of the hardest things to do is to admit that the medication you have worked so hard to develop does not do the thing you wanted it to do — or that it has side effects that are unacceptable and so won’t ever be useful. It’s important for scientists (who are regular people, after all) to build safeguards into their trials to help prevent this bias from slipping in and affecting their decision-making.
It’s also important to have someone else review the data – preferably someone who is invested in the field and so is familiar with the general shape of the terms you’re going to be throwing around (nothing gets in the way of critically analyzing a paper by having to go look up what “in S-specific CD4+ Th1 and Th2 cells and in CD8+ T cells” means) – to look for issues with the study design, the statistical analysis, and the conclusions that you’ve drawn. It turns out that double-checking your work is super important!
The process of double-checking scientific work is called peer review. In general, the medical journals that doctors rely on for their scientific information are referred to as peer-reviewed publications, meaning that any paper submitted to that journal goes through a peer review process before it can be published. It adds a layer of extra trust to the results of the paper — but it is not foolproof, and journals have been known to retract papers if it turns out the information they contain is inaccurate or misrepresented.
The Emergency Use Authorization (EUA) is another peer-review tool that allows the rapid-but-provisional approval of a drug, device, or intervention. Normally, the FDA review process takes about 10 months, as the agency reviews all of the available information and independently evaluates the benefit the new drug will bring to medicine, as well as the risks it may pose. Under the EUA process (as we’ve seen) that 10 month timeline can be shortened to “days-to-weeks”. A product that is being submitted for EUA is generally something that is urgently needed and has relatively strong information supporting its safety and effectiveness.
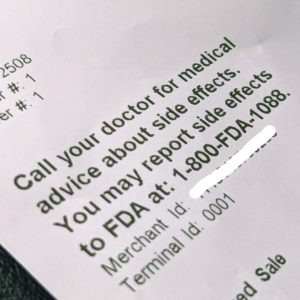
Because EUA approvals are based on a rapid review of early data, the manufacturers are required to provide ongoing updates regarding their continued study of the intervention. In the case of the coronavirus vaccines, the FDA has required a minimum of 2 months of data on safety following the final dose in the vaccine series, which is a much shorter followup interval than we normally see in a vaccine trial, and continued updates on their trial data over the next several years.
An EUA is a temporary authorization only; ultimately the vaccines that we are seeing will need to undergo a full review and obtain FDA approval, but their manufacturers will need to produce long-term data in order to obtain that approval. In the case of the coronavirus vaccines, the FDA has required a minimum of 2 months of data on safety following the final dose in the vaccine series, which is a much shorter followup interval than we normally see in a vaccine trial, and even the best physicists have not yet figured out how to manipulate time to get two years’ worth of safety data into two months.
Are you still with me? We’re into the home stretch.
Normally, once an intervention has completed 3 phases of trials and undergone full FDA approval, the drug companies begin manufacturing plans. In this case, manufacturers began ramping up to full-scale production of their vaccines in July, at the beginning of Phase 3 testing. That allowed Pfizer and Moderna to have doses of their vaccines ready to roll the day they were approved — but put them at significant financial risk if the trials were not successful.
So a lot of moving parts have been collapsed, abbreviated, combined, and restructured to allow this ultra-rapid timeline to proceed. When this happens, it requires everyone involved to be extra diligent about what they’re doing, how they’re analyzing it, and how they interpret the conclusions.
In the case of the coronavirus vaccine, the data we have appears solid, the endpoints and interim analyses were determined in advance, and the conclusions are supported by the data. That’s good. But the information we have right now is NOT final, and that is important to remember. The vaccine manufacturers have not closed their trials — they will be continuing to monitor trial participants for the next 2 years — and it’s important for people who are being vaccinated to participate in reporting their own experiences with the vaccine.
The more data we collect, the more we know. And the better our answers will be.